Understanding Full Hysterectomy Risks

When considering a full hysterectomy, it is crucial for patients to have an in-depth understanding of the potential risks and complications associated with the procedure. A hysterectomy, which is the surgical removal of the uterus, may sometimes also involve the removal of the cervix, ovaries, and fallopian tubes, depending on the individual's medical condition. This surgical intervention is often recommended for various reasons including Uterine Fibroids, Endometriosis, and certain types of cancer.
The Necessity of Hysterectomy
Before delving into the risks associated with full hysterectomy, let’s understand why this procedure is necessary. A hysterectomy can relieve chronic pelvic pain, heavy bleeding, and even life-threatening conditions. For many women, it represents a significant improvement in their quality of life.
Common Reasons for Hysterectomy
- Uterine Fibroids: Noncancerous growths in the uterus can cause pain, heavy bleeding, and other symptoms.
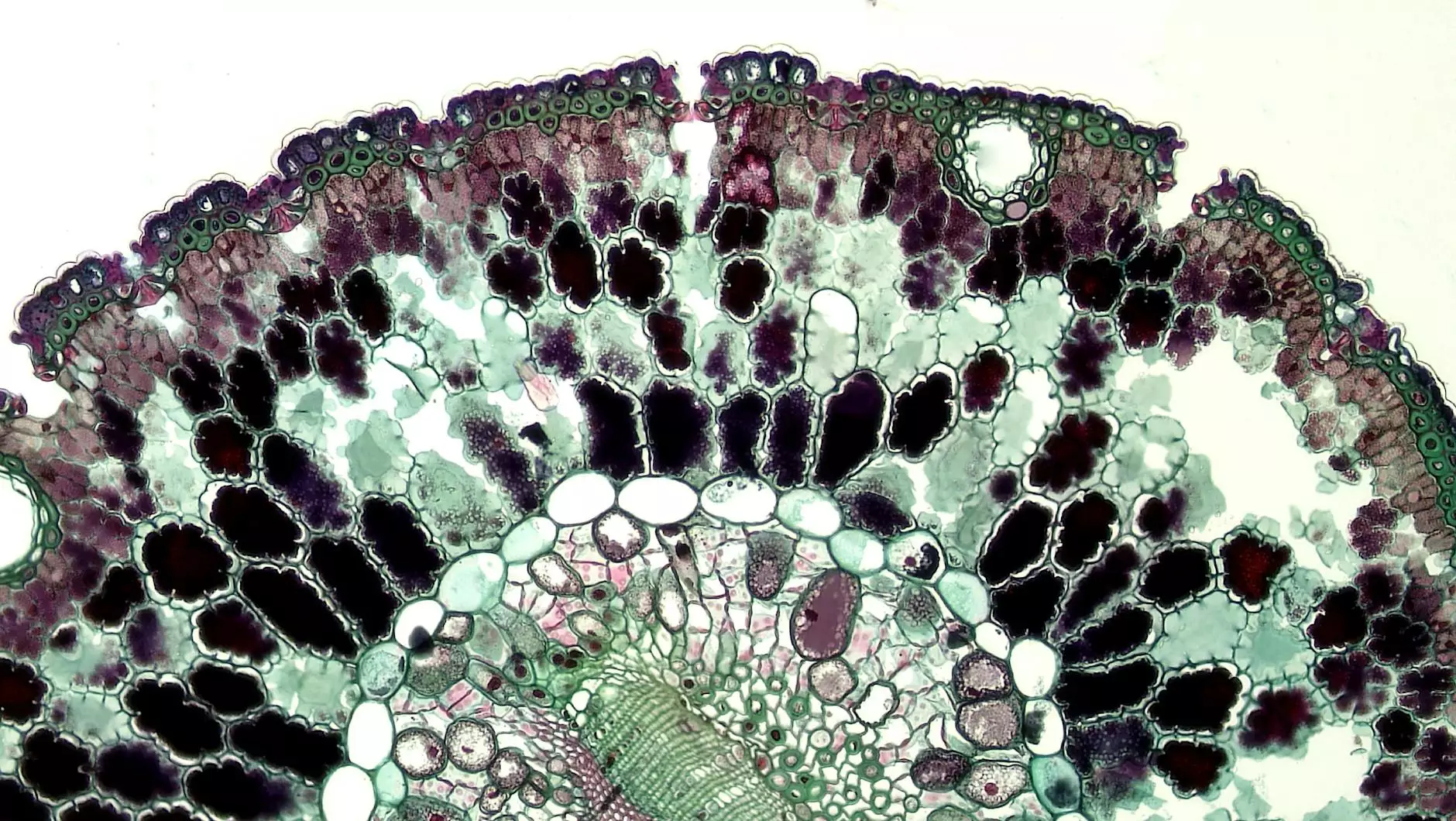
- Endometriosis: A painful condition where the tissue similar to the lining inside the uterus grows outside it.
- Uterine Prolapse: A condition where the uterus slips from its normal position into the vaginal canal.
- Cancer: In cases of uterine, cervical, or ovarian cancer, a hysterectomy may be necessary.
Potential Risks of Full Hysterectomy
Understanding the full hysterectomy risks is vital for informed consent. While many women undergo this surgery without significant complications, there are potential risks involved:
1. Surgical Risks
Every surgery carries inherent risks, including:
- Infection: Surgery can lead to infections at the incision site or internally.
- Bleeding: Excessive bleeding during or after the surgery may necessitate a blood transfusion.
- Anesthesia Complications: While rare, problems related to anesthesia can occur.
- Damage to Surrounding Organs: There’s a risk of damaging nearby organs such as the bladder or intestines during the procedure.
2. Long-term Risks
Aside from immediate surgical risks, women may face long-term complications following a hysterectomy:
- Hormonal Changes: If the ovaries are removed, this can lead to early menopause, resulting in symptoms like hot flashes, mood changes, and vaginal dryness.
- Bone Health Issues: Estrogen plays a crucial role in bone health. Its decrease post-hysterectomy may increase the risk of osteoporosis.
- Psychological Impact: Some women experience emotional changes post-surgery, including feelings of loss or depression.
- Sexual Dysfunction: Changes in sexual function may occur, including decreased libido or pain during intercourse.
3. Specific Complications
There are additional specific complications related to hysterectomy:
- Adhesions: Scar tissue can develop post-surgery, possibly leading to chronic pain or bowel obstructions.
- Urinary Issues: Some women might experience urinary incontinence or difficulty urinating.
- Pelvic Organ Prolapse: Subsequent to a hysterectomy, there might be an increased risk for other organs to prolapse.
Considering Surgical Options
Before progressing with a hysterectomy, patients should thoroughly discuss all surgical options with their healthcare provider. Alternatives like medication, hormonal therapies, or less invasive surgical approaches may also be considered and can sometimes mitigate the full hysterectomy risks.
Minimally Invasive Techniques
For some conditions, minimally invasive surgery (MIS) might be an option. Techniques such as laparoscopic hysterectomy can reduce recovery time and may result in fewer complications compared to traditional open surgery.
The Importance of Preoperative Care
Effective preoperative care is paramount in reducing risks associated with full hysterectomy. Prior to undergoing the procedure, patients should:
- Discuss Medical History: Provide a complete medical history, including all medications and supplements.
- Be Aware of Risks: Understand all potential risks and benefits, allowing for informed decision-making.
- Engage in Prehabilitation: Some benefits may be gained through physical therapy or lifestyle changes prior to surgery.
Post-Operative Care and Recovery
After a full hysterectomy, proper post-operative care significantly influences recovery outcomes. Patients should:
- Follow-Up Appointments: Regular follow-ups with the doctor are critical for monitoring recovery and managing any complications.
- Exercise and Mobility: After recovery, gentle exercises can promote healing and overall physical health.
- Manage Pain: Report any excessive pain to the healthcare provider to adjust pain management protocols as needed.
Emotional and Psychological Support
Women undergoing a full hysterectomy might require emotional and psychological support. Connecting with support groups and counseling services can be instrumental in navigating the emotional landscape that follows major surgical procedures.
Conclusion
In conclusion, while a full hysterectomy can be an essential and life-improving procedure for many women, understanding the full hysterectomy risks involved is imperative. Engaging in discussions with healthcare providers about individual conditions, alternative treatments, and thorough preoperative and post-operative care can fully equip patients to make the best healthcare choices tailored to their individual needs. The journey post-hysterectomy may be challenging, but with the right approach, many women find renewed strength and empowerment in their health and well-being.
For more information regarding full hysterectomy and related health services, please visit Dr. Seckin's official website.